12 Simple Ways to Prevent Memory Loss as You Age: a Functional Medicine Approach
It’s a common worry that faces millions as they age - what if I start to develop memory loss? Memory loss disorders are a particularly dreaded enemy. My patients who do have dementia all have different experiences with it. Some of my patients recognize their cognitive challenges, yet some are unaware that their memory is diminishing. It’s all a spectrum. Regardless of how people experience their dementia, it’s an incredibly challenging road to travel for the patient, loved ones, and caregivers.
Two basic tenants are true when it comes to combating memory loss. First, it’s important to try and cultivate inner peace if you have a memory loss disorder. Second, it’s important to practice moment-to-moment grounding exercises. Developing inner and outer resources, such as building stress resilience is crucial.
It’s also vital to understand that, contrary to common belief, our brains are malleable organs with the life-long ability to form new pathways, change, and grow. You can integrate tactics into your life that can help you prevent memory loss as you age, as well as during the early stages of Alzheimer’s and dementia.
What are Modifiable Risk Factors for Alzheimer’s?
Known risk factors for Alzheimer’s disease and dementia are surprisingly modifiable. This means there are actually many things you can do earlier in life to prevent the onset of these diseases.
A study done in 2020 by the Lancet Commission, alongside other studies, identified numerous modifiable risk factors for Alzheimer’s and dementia. This specific study includes many contributing factors like exposure, environmental toxins, latent viruses, a history of chronic stress, and emotional trauma.
Additionally, in 2014, a pivotal study was published by Dr. Dale Bredesen. This study highlighted many biological risk factors of Alzheimer’s disease. In turn, his findings seeded an entire movement in neuropsychology. The movement now understands that a functional medicine approach can help identify the root causes of cognitive decline to prevent and treat dementia.
Some Alzheimer’s Disease Modifiable Risk Factors:
-
Avoid alcohol
-
Stop (or don’t start) smoking
-
Decrease exposure to air pollution (including second-hand smoke)
-
Decrease midlife obesity
-
Reduce hypertension
-
Avoid head injury and treat any concussions quickly
-
Treatment of hearing impairment (use of hearing aids and avoidance of excessive noise levels)
-
Analyze prescription medication with MD or DO (polypharmacy)
-
Improve sleep quality, watch for sleep apnea
-
Develop muscle strength
-
Improve cardiovascular health
How can Maintaining a Healthy Mind Help With Alzheimer’s?
When we think about maintaining brain health, we often don’t jump right to the ideas of mental health management and emotional regulation. However, science shows that emotional health is intimately tied to overall brain health. For example, depression and other mental health disorders are often associated with Alzheimer’s disease.
Understanding and regulating your emotions is actually a huge part of developing a healthy mind. You can maintain and enhance brain and mental health by increasing your neuroplasticity and strengthening the neural pathways in your brain as you age.
The good news is, we have access to this glorious plasticity from the moment we take our first breath until the moment we take our last. It’s a stark misconception that our brains are only malleable in our youth. A study conducted by the National Library Of Medicine used neuroimaging to reveal persuasive evidence of plasticity even as the brain ages, including during the early stages of dementia. This means that our brains are malleable all the way up until the end of our lives - isn’t that a beautiful truth?
This information provides a great well of hope for those battling Alzheimer’s disease or dementia. It signifies that we may actually have more control over our mental acuity in the early stages of deterioration than is often first perceived.
What are Daily Practices to Prevent Memory Loss?
In our practice, it’s important to me to always encourage patients to take tangible, daily actions to keep their minds active, engaged, and inquisitive. To lock in these habits, I recommend that you have one place where you can write down and schedule your brain health activities. Schedule these simple habits into your daily life!
Include These in Your Daily Life to Prevent Memory Loss:
-
Healthy eating (mostly plants)
-
Exercise each day, and mix up your routine
-
Meditation (there are all kinds, pick your favorite!)
-
Therapy (talk to someone about things you rarely talk about)
-
Activities you enjoy, as well as some new ones
-
Music and other creative outlets
-
Other mentally stimulating activities, challenge yourself often
-
Attain higher levels of education/stimulation
-
Engage with others / increase social connections
-
Get sufficient and restorative sleep
Aging shouldn’t be something we fear, but something we embrace as we wisen and schedule in the work (and play) to stay emotionally and cognitively healthy. In our clinic, we call a fully healthy lifespan a “healthspan”: a life that is both long AND healthy!
Self-Care for Caregivers: 10 Tips for Caring for a Loved One with Dementia
Self-Care for Caregivers: 10 Tips for Caring for a Loved One with Dementia
Caregiving for a loved one with dementia can be an emotionally overwhelming and physically demanding job. As a caregiver, it is easy to put all of your time and energy into taking care of your loved one, but it is important to remember that taking care of your emotions and your nervous system are just as crucial. Focusing on your overall health ought to be a priority, as self-care for caregivers is care for the receiver too.
Effects of Caregiving on Caregivers
Caregiving can quickly lead to burnout, stress, depression, and a compound of health issues that arise from prolonged stress & poor mental health. Many caregivers report insufficient time to sleep, exercise, or otherwise maintain healthy habits, putting them at risk for developing chronic illness. When you’re a caregiver, your nervous system is often in active threat response because you are focusing on someone else’s safety. That can take a toll. In fact, surveys reveal that nearly half of caregivers have two or more chronic diseases—some of which are themselves risk factors for dementia.
Why Is Self-Care Important?
Self-care for caregivers is essential to their continued health and ability to care for their loved one long term. It is important to recognize that taking care of yourself is taking care of your loved one: when you prioritize your own health and well-being, you are better equipped to provide quality care to your loved one with dementia.
Barriers to Self-Care for Caregivers
There are many logistical barriers that can get in the way of sufficient self-care for caregivers, but oftentimes, it is emotional resistance and contradicting beliefs that keep one from pursuing solutions and creating time for themselves.
For example, these are some commonly expressed worries among caregivers:
- It is selfish of me to prioritize my own health.
- Caring for myself is neglecting my loved one.
- I fear I will do a poor job if I am not always providing care.
- If I ask for help, it will reveal that I am an inadequate caregiver.
- I am responsible for my loved one’s health and quality of life.
- Only if I do everything right will my loved one be okay.
- I owe all of my time to my loved one; that is what they deserve/what I promised them.
- My family will think less of me if I take time for myself.
If you have had any of these thoughts or worries as a caregiver, you are not alone. It is natural to feel the weight of your loved one in these ways. However, it is important to understand that these are misconceptions that can increase anxiety and make it impossible to give yourself the care you need.
Before you can take steps toward sustainable self-care, it is important to identify mental barriers like these that might keep you from accepting care from yourself and others. Once you do, here are 10 more steps you can take toward better self-care and therefore better care for your loved one.
1. Learn More about Dementia and Cognitive Decline
A pillar of self-care for caregivers is stress reduction, and one important, practical way to reduce stress is to take the time to learn about cognitive decline and dementia and how it is affecting the behaviors, emotions, and abilities of your loved one. Whether they are experiencing early memory loss or late-stage dementia, it is helpful to understand what changes you can expect so that not only are you better equipped to provide caregiving support, but also prepared to process your own emotional responses to these changes in someone you know and love.
2. Set Realistic Expectations
Don’t overwhelm yourself with an overloaded to-do list. As a caregiver, you want the best for your loved one, and you likely have high expectations for the care you provide. It is easy for these high expectations to turn into unachievable goals, so remember:
- Setting your expectations too high is only setting yourself up for disappointment.
- Your productivity is not a reflection of your love, dedication, or adequacy as a caregiver.
Instead, start by writing down all your goals. Then, prioritize these goals based on what matters the most to you and establish timelines that feel manageable. If the tasks that absolutely must be done today do not feel manageable, ask for help.
3. Accept Help
Asking for and accepting help is one of the most important, yet often most difficult, acts of self-care for caregivers. As a caregiver, you deserve support just as much as the person you are caring for, and you may be surprised at how willing and eager others are to help.
Plus, by delegating tasks that others could do, you can free up your time and energy to focus on the most important aspects of caregiving, like spending time with your loved one and taking care of your own health. If you are struggling to ask for help, there are a few things that might help:
- Firstly, remember that people want to help and that asking for help is not weak or shameful.
- Make a list of people in your social circle who have offered to help, categorizing their offers as practical, emotional, or spiritual.
- Categorize your needs in the same way, and set priorities on your tasks to inform clear and direct communication.
4. Take Breaks
Self-care does not have to happen all at once at the beginning or end of your day. Self-care is most impactful when it appears intentionally throughout your day.
It can be as simple as taking a walk around the block or sitting alone for a few minutes between activities, but these little moments of rest are essential in preserving your energy and managing stress throughout the day. Though it may seem obvious, interrupting the day with breaks requires intention. You may be surprised at how little you pause during the day when you don’t actively try.
5. Maintain Healthy Habits
The health of caregivers is integral to the health of care recipients. When we are busy, distracted, or overwhelmed, sometimes the first things to go are the most essential, so a core aspect of self-care for caregivers is being intentional to maintain a few basic habits that are vital to long-term health, and brain health in particular. Something we always talk about. Focus on our 6 Pillars of Brain Health and do things like:
- Sitting down and eating nutritious meals that support your brain and overall health, such as vegetables and protein-rich foods
- Exercising for at least 30 minutes a day, five days a week—especially in nature where exercise can double as a therapeutic reset
- Ensuring at least 7 and a half hours of restful sleep each night, which is integral to so many of the body’s vital functions
Many caregivers have to work extra hard to maintain their health, and supplementation offers one way to provide your body additional support and to sustain healthy aging. Studies have shown, for example, that Vitamin D3, Folate, Vitamin B-12, Vitamin B-6, and Choline can help with longevity and support brain health as well. Making brain and emotional health your priorities are some of the ways you can care for yourself.
6. Practice Gratitude
Practicing gratitude—thinking of one thing you’re grateful for every morning or writing a letter of appreciation, for example—can help you recognize the positive aspects of your caregiving journey, as well as grow your appreciation for yourself as a caregiver.
A gratitude practice does not have to be forced or falsely positive; it simply encourages you to direct your attention at the things you appreciate in others and yourself, in order to feel more fulfilled and energized. This can help to build your self confidence, improve your relationship with your loved one with dementia, as well as help you feel more connected to the people around you for a stronger sense of support and belonging.
7. Remember to Breathe
Deep breathing is a powerful tool in reducing stress and anxiety, improving sleep, and promoting overall well-being. Deep breaths can increase the oxygen flow in your body, which can help you feel more relaxed and focused.
The 4-7-8 breathing technique, developed by Dr. Andrew Weil, is a simple, quick, and deeply relaxing exercise that can easily be integrated into your routine, or practiced over a break, to breathe calm into your day.
8. Take Time for What You Love
Creating time and space for hobbies and personal growth can be a particularly challenging aspect of self-care for caregivers. As nonessential activities, it can be easy to feel that recreational, creative, or educational activities are overly indulgent.
But in fact, these activities are crucial to reducing stress, sustaining a strong sense of purpose and selfhood, and maintaining sharp cognitive function, which is important not only to the longevity of your own brain health, but your ability to provide the best possible care to your loved one, too.
9. Stay Connected
As a caregiver, it can be easy to feel isolated and disconnected from the world outside of your caregiving relationship. For this reason, it is particularly important to invest time in your other relationships with friends and family. Whether a friend who always makes you laugh or a family member who is a great listener, staying connected with loved ones can help you feel more balanced and energized.
Additionally, dementia caregiver support groups can provide a safe and supportive space for you to share your experiences and connect with others who are going through similar challenges. Talking with others who understand what you are going through can help alleviate feelings of isolation and provide valuable insights and tips for coping with the stresses of caregiving.
10. Get Support
In addition to support groups, getting mental health support from a professional can be beneficial for managing stress and maintaining emotional wellbeing. Emotional resilience psychotherapy is a form of therapy that Dr. Rusk focuses on at the Brain and Behavior Clinic. It is all about healing emotional trauma responses to improve cognitive and behavioral symptoms. This therapy can help caregivers cope with the emotional toll of caregiving and improve their overall quality of life.
It is essential to remember that self-care is an act of care for your loved one too, and that receiving and seeking support is not a sign of weakness.
If you are a caregiver for a loved one with dementia, reach out to the Brain and Behavior Clinic, and work with our team of experienced therapists, neuropsychologists, and other brain health specialists to develop personalized brain health plans that optimize your cognitive health and the overall wellbeing of your nervous system and that of your loved ones.
Dementia Prevention: How to Reduce Risk Factors for Cognitive Decline
Dementia Prevention: How to Reduce Risk Factors for Cognitive Decline
As we age, physical changes occur in our brains and impact our cognitive function. Some of these changes, like occasional forgetfulness, are normal for some people as they age, but progressive or persistent loss of memory, or other cognitive functions, are not.
Major cognitive decline with aging often indicates some type of neurological change which can be because of a neurodegenerative disease which can often progress to dementia. The most common of the dementias are Alzheimer’s disease (AD) and vascular dementia, and they can often exist together.
Who Is at Risk?
There are a few known risk factors for dementia that are not within our control. These include:
Age
While dementia is not a normal part of aging, it primarily affects people older than 65 years. While cognitive decline does occur in younger people, dementias rarely do. Approximately 1 in 9 people over the age of 65 are living with Alzheimer’s disease, and among these, 73% are 75 years or older.
Genetics
Presenilin mutations and the APOE4 gene are genetic factors which have been linked to the development of Alzheimer’s disease. Fortunately, even in the presence of these genes, research shows that disease-related cognitive decline can be slowed down, even halted in some cases, and that dementia can be prevented through early interventions and lifestyle factors that are within our control. Many of the providers we work with at the Brain and Behavior Clinic are trained by Dr. Dale Bredesen who developed the Bredesen Protocol which addresses root biological and lifestyle causes for cognitive decline.
Understanding and Modifying Risk Factors
Hearing + Vision Impairment & Cognitive Decline
Understanding the Risk
The exact mechanisms linking hearing and vision impairments to cognitive decline are not yet fully understood, but we do know that decrements in auditory acuity decrease brain processing in the temporal lobes in the brain. While some research suggests that these impairments directly affect the brain’s function, others suggest that hearing and vision impairment contribute to feelings of social isolation and reduced stimulation of the brain, thus resulting in cognitive decline.
Reducing the Risk
While there is a significant link between mid-life hearing impairment (2020 Lancet Commission report) and later risk of cognitive decline, this is one of the easiest risk factors to modify for dementia: optimizing hearing and vision with the use of hearing aids and vision correction can substantially reduce the risk.
Diet & Cognitive Decline
Understanding the Risk
A diet that is high in saturated fat, sugar, and salt can cause a number of health problems that have been identified as risk factors for dementia, including:
- Inflammation
- Obesity
- Cardiovascular problems like:
Reducing the Risk
Eating a diet that is low in saturated and trans fats and rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk of cardiovascular illness as well as reduce inflammation more generally. This benefits the immune system. Limiting salt intake can further help to maintain healthy blood pressure, which reduces the risk for dementias caused by cerebrovascular changes. Additionally, a balanced diet can optimize the diversity of the gut microbiome which supports stress resilience.
Alcohol Use & Cognitive Decline
Understanding the Risk
Excessive alcohol consumption can lead to various health problems, including high blood pressure and heart disease, which are themselves risk factors for dementia. Alcohol itself is a neurotoxin, and excessive use of alcohol impacts the health of neurons. In the Blue Zones, where the world’s greatest number of centenarians live, alcohol use is small and restricted to when people are eating and socializing.
Reducing the Risk
If you do drink alcohol, it is important to limit consumption, and if you drink wine it is best to drink red wine made with organic grapes. While the amount of recommended alcohol use varies, many experts consider one drink per day to be the threshold under average health circumstances. If you are unsure about your level of consumption, talking to your doctor to get a better sense of your personal threshold might be a good first step; and if you have cognitive problems, drinking any amount of alcohol is too much!
Smoking & Cognitive Decline
Understanding the Risk
Smoking has various toxic effects, including the formation of plaque in the blood vessels, which increases the risk of vascular diseases. Many studies have shown that smoking—and second-hand smoke—can directly cause cognitive decline as well. One study, for example, found that in women aged 55–64 years, exposure to second-hand smoke was associated with greater memory deterioration.
Reducing the Risk
If you are a smoker, quitting smoking is one of the most important steps you can take to reduce your risk of cognitive decline and maintain healthy aging. And it is not too late to quit:
One longitudinal study comparing 50,000 men found that those who had stopped smoking for more than four years showed a significantly lower risk of developing dementia than those who had continued smoking.
Air Pollution & Cognitive Decline
Understanding the Risk
Air pollution is increasingly being recognized as a risk factor for cognitive decline and dementia. Numerous studies have linked high concentrations of nitrogen dioxide and fine particulate matter from traffic exhaust and residential wood burning with an increased incidence of dementia. These pollutants can penetrate the blood-brain barrier and cause inflammation and oxidative stress, which are both linked to cognitive decline.
Reducing the Risk
While you may not always be able to control the pollution in your external environment, there are steps you can take to avoid your exposure to it:
- Get in the habit of checking local air quality indexes to avoid exposure to high toxicity levels.
- Avoid busy roads when possible, and when driving in high-traffic areas, avoid AC modes that draw outside air into your car.
- Use an air filter in your home, and limit your use of wood-burning stoves and fireplaces.
Mental Health & Cognitive Decline
Understanding the Risk
Our emotional wellbeing is directly tied to our cognitive health in both temporary and long-term ways. Chronic stress and anxiety can lead to the production of stress hormones, like cortisol, which can damage brain cells and accelerate the aging process. Similarly, depression can lead to inflammation in the brain, which can cause cognitive decline over time.
Reducing the Risk
For those struggling with depression or anxiety, psychotherapy is an instrumental tool in managing symptoms and supporting healthy cognitive aging. Healing chronic stress by working on old traumas is very important when addressing dementia prevention, and treatment. In addition to treating emotional disorders, you can proactively build emotional resilience through practices like:
- Meditation or other mindfulness practices
- Regular exercise, especially in nature
- Regular social engagement to maintain strong relationships
- Sharing difficult feelings with people who you trust
- Working through grief, shame, and self-judgment
- Building a trusting relationship with a psychotherapist
Sleep & Cognitive Decline
Understanding the Risk
Sleep deprivation has been linked to a wide range of physiological changes that could contribute to cognitive decline, as well as other known risk factors, such as:
- An increase in β-amyloid (Aβ) proteins, which are associated with Alzheimer’s disease
- Inflammation
- Cardiovascular disease
- Hypoxia (sometimes associated with obstructive sleep apnea) which can damage brain cells and contribute to cognitive decline
Reducing the Risk
A couple of ways to ensure sufficient amounts of sleep to reduce sleep-related risk factors include:
- Setting consistent routines to help you make this aspect of health a priority
- Curating an environment that is optimized for comfort and sleep needs
- Investing time in your emotional health to reduce stress and support better sleep
For people who have sleep disorders such as sleep apnea, it is important to seek treatment to support sufficient sleep and promote long-term cognitive health. Many patients who have cognitive decline and sleep apnea benefit from using a specially fitted CPAP machine.
Brain Injury & Cognitive Decline
Understanding the Risk
Brain injury can cause inflammation, oxidative stress, and neuronal damage, which can eventually lead to the development of dementia. The risk of injury-related dementia increases with the severity of damage, the age at which the injury (or injuries) are sustained, and the frequency of traumatic brain injury or concussion.
Reducing the Risk
If you have sustained a mild brain injury, there is often so much you can do to reduce its lasting impact on your brain health—especially when you act early. It is important to seek medical attention immediately and to receive a customized treatment plan.
Of course, the best way to reduce injury-related risk is to actively prevent head injury by taking steps like:
- Engaging in road-safe practices like wearing your seatbelt, ensuring a well-maintained vehicle, and only driving when you are well rested and sober
- Always wearing the proper protective gear like helmets while engaging in high-risk sports or other activity like biking or skiing
- Taking precautions to prevent falls, like installing handrails, removing tripping hazards, and improving lighting
Exercise & Cognitive Decline
Understanding the Risk
Lack of Physical Exercise:
Multiple studies, including longitudinal studies spanning 1–21 years and a HUNT study of about 30,000 participants demonstrate a link between MVPA (moderate to vigorous physical activity) and reduced risk of dementia.
Lack of Mental & Social Stimulation:
Lack of social activity is also considered a risk factor for cognitive decline. Social isolation can lead to a decrease in mental stimulation, which may have negative effects on cognitive functioning. A systematic review and meta-analysis of 51 longitudinal cohort studies found that high social contact was associated with better late-life cognitive function. Retirement is only beneficial for cognitive function if you have other ways to remain engaged with novelty and new stimulating activities.
Reducing the Risk
While the nature of these activities will likely fluctuate as you age and change, it is important to maintain regular stimulation of your brain and to regularly exercise enough to get your heart rate up for at least 160 minutes per week. Here are a few ways to maintain social, mental, and physical activity:
- Attend group exercise classes.
- Engage with your community by attending local events, volunteering, or joining a club or meet-up group.
- Learn a new skill or set of knowledge, like a second language.
- Go dancing or play board games with friends.
- Do online cognitive training daily.
Preventing Cognitive Decline with the Brain & Behavior Clinic
Taking early action is the best way to prevent dementia, and a brain check-up is a great place to start. At the Brain and Behavior Clinic, we offer a Healthy Brain Check-up, which involves a personalized scientific evaluation of your unique history and emotional, biological and cognitive profile. We do a careful analysis of your sleep, exercise, nutrition, stress, and other lifestyle patterns and then individualize your neuroplasticity plan.
With this knowledge, we can help you understand and mitigate your personal risk factors and coach you to prevent Alzheimer’s or help you optimize your peak cognitive performance. Trauma healing and stress optimization are the goals when it comes to feeling hopeful about your health and good about yourself.
The Healthy Brain Program
Following your personalized functional medicine brain check-up, our doctors will develop a customized program, including cognitive training, lifestyle coaching, and wellness therapies, to support your brain’s healthy aging and provide targeted dementia prevention. We treat many patients who have chronic environmental illness as well.
Customized to the individual’s needs, our program can include:
Cognitive Training
- HeartMath: a type of biofeedback that helps you learn how to regulate your heart rate variability to improve cognitive function and emotional regulation
- Neurofeedback: a type of brain training that helps you learn how to regulate your brain activity for improved cognitive function
- Meditation training: a technique that promotes relaxation, stress reduction, and improved cognitive function through focused attention on the present moment
Lifestyle Coaching
- Nutrition treatments
- Sleep and movement support
- Mindfulness practices
Trauma and Resilience Therapies
- Nervous system psychotherapies informed by
- Applied Polyvagal Theory
- Somatic Psychotherapies
- Embodiment practices
- Breathwork Practices
- EMDR
- Brainspotting
- Somatic Experiencing
If you want to sharpen your mind and deal with healing trauma, depression, fears, anxiety or other mental health issues, please contact us at the Brain and Behavior Clinic.
If you or someone you care about is at risk for dementia or is struggling to manage cognitive or trauma-related symptoms with chronic illness, we are here to help. Contact our clinic anytime.
Brain Injury After a Car Accident: What You Need to Know
Brain Injury After a Car Accident: What You Need to Know
Car accidents can be devastating and life-changing events which can result in financial loss, trauma, and serious or life-threatening injury—particularly traumatic brain injury (TBI).
Unfortunately, car accidents are not rare. In 2020 alone, there were over 5 million auto collisions reported in the United States, and these accidents continue to be a leading cause of TBI.
What to Do If You’ve Been in a Car Accident
Given the prevalence of car accidents and the potential severity of related brain injuries, it is critical to know how to respond if you have been in an accident.
1. Get Examined Immediately
If you have been in a car accident, it is crucial to seek medical attention as soon as possible, even if you do not feel any immediate pain or symptoms. For some brain injuries, like concussions, symptoms can take hours or even days to set in, especially if they are masked by other symptoms or pain.
2. Seek Diagnostic Evaluation at a Hospital
It is important to get a comprehensive evaluation by a medical professional who has experience diagnosing and treating brain injuries, as these injuries can be highly complex and can have long-term consequences if left untreated.
3. Document Your Symptoms
Keeping a detailed record of your symptoms, including when they started, how severe they are, and how they have affected your daily life, can help your doctor make an accurate diagnosis and determine the best course of treatment for your brain injury.
4. Seek Follow-up Care as Necessary
Brain injuries can have prolonged effects on your physical, emotional, and cognitive wellbeing. If you have noticed significant changes in your moods or decreased cognitive function, you may need ongoing treatment from a neuropsychologist or other brain health specialists to manage your symptoms and promote continued healing.
5. Get the Support You Need to File an Insurance Claim
Insurance claims can be filed not only for vehicle-related expenses, but for injury-related expenses as well, such as medical bills, ongoing treatment expenses, lost quality of life, or lost income resulting from the inability to work. Though common, car-accident-related brain injuries are complex, and to understand their cause and scope often requires specialized expertise.
For this reason, many lawyers specialize in brain injuries, often talking with neuropsychologists to understand the impact of their client’s injury and the treatment necessary, and to help their client obtain the appropriate compensation they deserve for their injuries.
Brain Injuries
The brain is a delicate and complex organ that can be injured in a variety of ways and to many different degrees during a car accident or other trauma. Regardless of the type or severity of brain injury, it is important to note that all of them can have significant effects on a person’s life and long-term health.
Not everyone who is involved in an automobile accident or injury suffers a concussion or traumatic brain injury, and if you do suffer such an injury, the odds are that you will fully recover within a few days or months. But sometimes problems can linger. Fortunately help is available.
Concussion
The most common type of brain injury, a concussion occurs when the brain is jolted or shaken inside the skull due to impact or other physical forces. In the case of a car accident, this could happen when the head is thrown around in a collision or when the head strikes a hard object like a steering wheel, dashboard, or window.
Brain Contusion
A brain contusion refers to a bruise on the brain. As with a concussion, brain contusions can occur when the head directly hits a hard surface, like a side window or the roof of the car. Often, they result from a violent jolt during which the brain slams against the inside of the skull.
Skull Fracture
If the head is hit with enough force, the skull bone can fracture, or crack. Typically if a fracture is sustained, the brain also incurs a concussion and brain contusion. A fracture could occur when the head smacks against the car or when the skull is penetrated by an object.
Coup-Contrecoup
Coup-contrecoup injuries occur when there is an impact to one side of the head so severe that it causes the brain to hit the opposite inside of the skull, resulting in two separate injuries on either side of the brain. This could happen during a car accident that is particularly violent, like a T-bone or rollover collision.
Brain Penetration
A severe form of traumatic brain injury, brain penetration injuries occur when extreme force causes an object to cut through the skull and enter the brain. Brain penetration injuries could happen during a car accident when objects from inside or outside the car, such as shattered glass or metal debris from the car, penetrate the skull.
Symptoms of Car Accident Brain Injury
The symptoms of a traumatic brain injury (TBI) can vary significantly based on the type and severity of the injury. Moderate to severe TBIs, such as some brain contusions or penetrating injuries, can cause symptoms like major memory loss, seizures, permanent disability, or even death.
Mild TBIs, most commonly concussions, may cause temporary symptoms, prolonged symptoms, or if untreated, result in lasting damage. Whether or not symptoms are present, it is recommended that you seek medical attention immediately after an accident during which you may have injured your brain, as early diagnosis and treatment can significantly improve the outcome of a TBI.
Common Physical Symptoms:
- Headaches
- Dizziness
- Blurred vision
- Sleep problems
- Ringing in the ears
- Balance difficulties
- Significant fatigue
Common Emotional or Behavioral Symptoms:
- Irritability
- Decreased patience
- Frustration
- Driving fears
- Low motivation
- Anxiety and worry
- Personality changes
- Sadness and depression
Common Cognitive Symptoms:
- Attention and concentration problems
- Slowed thinking
- Memory difficulties
- Mental inefficiency
- Tendency toward cognitive overwhelm
- Speech and word-finding problems
- Limited strategic or organizational thinking
Treatments Available
Treatment depends on the type and severity of brain injury incurred; but typically, comprehensive treatment begins with a diagnosis of the specific injury and addresses the unique physical, emotional, and cognitive symptoms experienced by the patient, as well as the disruptive problems these symptoms can cause, such as:
- Driving anxiety
- Inefficiency at work
- Inability to manage responsibilities beyond work, like volunteering, household chores, and friendships
- Guilt about the decreased ability to function
At the Brain and Behavior Clinic, our initial evaluation involves a comprehensive 2–3 hour appointment with one of our neuropsychologists. Following this, our doctors and specialists work together to create an individualized treatment plan which, depending on the patient, could involve:
- Short-term trauma psychotherapy to address any stress or driving anxiety the person may be experiencing following their crash
- Occupational therapy to develop compensation and limit-setting strategies for managing the many daily responsibilities they have and which they are having trouble fulfilling
- Medication recommendations, often to aid sleep or improve cognitive abilities
- Referrals to trusted clinicians for:
- A vision evaluation
- A vestibular evaluation,
- Nutritionist care to ensure the brain is supplemented with the proper foods for enhanced recovery
If you have been in a car accident and may have suffered a traumatic brain injury, whether or not you have already received a diagnosis, call our clinic. Our experienced doctors can help you understand any brain injury you may have, and if relevant, help you get started with the right treatment for your specific set of circumstances.
A Parent’s Guide to Sports-Related Concussion: Prevention & Safety Tips
A Parent’s Guide to Sports-Related Concussion: Prevention & Safety Tips
A concussion is a form of mild traumatic brain injury which can be caused by any impact to or forceful movement of the head. Though it is considered a “mild” TBI, concussions are very serious—especially for children and young adults whose brains (up until their early 20s) are still developing and therefore are more susceptible to long-term damage.
While sports benefit kids’ development in a number of ways, they also pose the greatest risk for concussions in young people. That’s why it is essential that parents, coaches, trainers, and young athletes themselves take all possible precautions to avoid injury, as well as understand signs, symptoms, and treatments in the event a concussion is sustained.
5 Ways to Help Prevent Sports-Related Concussions
- Ensure your child has the proper equipment.
Before your child begins playing, check that they have the appropriate gear—especially a helmet. In addition to being sport-specific, a helmet should be:- The right size and fit
- Certified by the appropriate association: NOCSAE or ASTM
- Replaced when damaged or outdated (Standard recommendation is to replace after about 5 years, unless damaged earlier.)
- Ensure your child is playing in a safe environment.
Falls are the most common cause of concussion in sports. To reduce fall risk, make sure all practice and game areas are ready for play: fields should be hole- and rut-free, and courts should be level and free of cracks or bumps. Additionally, the risk of injury can be limited by avoiding unnecessarily hard surfaces like concrete, and instead playing only on softer surfaces like grass fields, tracks, and wooden courts. - Ensure your child knows the rules and proper sports techniques for avoiding injury.
Though safety techniques should be taught by your child’s coach, you can help by ensuring they understand their coach’s instructions and by teaching them the basics before they begin. For example, the head-up technique helps athletes avoid unnecessary helmet-to-helmet contact, and using the forehead rather than the crown helps ensure a safe headbutt in soccer. - Ensure that all coaches and referees are following proper procedures, like:
- Enforcing the rules and gear-wearing for all players
- Teaching and reinforcing the importance of safe playing techniques
- Practicing on safe grounds, accompanied by someone who is trained in injury response
- Incorporating muscle training of the shoulders and neck
- If you see your child get hit in the head or otherwise injured while playing, ensure they are immediately removed from the game.Once removed from the game, make sure your child gets checked for a concussion by a qualified athletic trainer or school nurse; and if necessary, take them to the hospital.
How do I know if my child has a concussion?
A person does not need to lose consciousness to have sustained a concussion, and their symptoms may not set in right away. That is why, if your child has been hit in the head, it’s important to observe them closely for at least 48 hours.
Young children may have trouble communicating their symptoms. They may only manage things like, “I don’t feel right” or act out more than usual. Additionally, older youth may intentionally choose not to report their symptoms in response to social or performance pressures, like letting down their team or missing college opportunities.
For these reasons, it is especially important to know the signs and symptoms of a concussion. If you are concerned that your child is refusing or struggling to convey their symptoms, here are some things you can look for:
- Slowed reaction times
- An inconsistent gait
- A sudden change in habits
- Loss of Interest in usual activities
- Irritability
- Lethargy
- Unreasonableness
- Reclusiveness
- Reports of behavioral, emotional, or cognitive changes from teachers or friends
What should I do if I suspect my child has a concussion?
If you suspect your child may have a concussion—whether or not symptoms are apparent—it’s best to get them seen by your doctor as soon as possible. If your child begins to exhibit any of the following symptoms, they should be taken to the hospital right away:
- Loss of consciousness
- Imbalance
- Vomiting
- Change in vision
- Unequal pupils
- Slurred speech
- Confusion
- Rapidly worsening symptoms
How can I treat my child’s concussion?
For the first 48 hours following injury, here are a few ways to ensure your child’s safety and support their healing process:
- Keep a close eye: don’t leave your child alone, and check on them throughout the night.
- Sleep is good! You don’t need to wake them throughout the night, but check that they are breathing and sleeping restfully.
- Do not give your child aspirin or ibuprofen; opt for acetaminophen to manage headaches for the first 48 hours.
- Help them rest: create a comfortable environment without bright lights or loud sounds, and discourage them from stimulating activities like using the computer, texting or scrolling through their phone, playing video games, or watching tv.
- Help your child avoid physical and mental exertion, like homework: if they have homework, help them make a plan to talk with their teachers.
- Don’t isolate your child entirely: minimal social contact, like talking with a friend or sitting with family is healthy.
- Take your child to the doctor for a check-up.
A child’s recovery can take anywhere from minutes to months, depending on several factors like age, extent of impact, previous brain insults or injuries, and many other factors; and it can be difficult to know precisely when your child has fully recovered. Follow your doctor’s advice, and continue to observe your child until you see a consistent demonstration of their previous level of functioning.
Until then, here are some ways you can promote your child’s continued recovery:
- Ensure that your child is equipped to communicate with teachers regarding missed tests or homework and that they are given the appropriate school accommodations. (This may involve an IEP or 504 Plan.)
- Help your child achieve a balance between rest and pushing themselves.
- If they are struggling to sleep, talk to your doctor about supplements or medications or take other measures to aid your child’s sleep.
- Notice when your child is experiencing emotional overload or distress, and help them manage their emotions.
A good rule of thumb is that your child should be symptom-free for one week and demonstrate significant progress toward their usual cognitive and physical activity levels before they return to play. Until then, they should not return to their sport and should avoid:
- Excess screen time
- Bright lights
- Strobe lights at school dances or parties
- Listening to loud music or music through headphones
- Concerts
- Pep rallies
While it is not possible to completely negate the risk of sports-related concussion, you can significantly reduce your child’s risk by practicing a few precautions, and you can further reduce the risk of lasting damage by understanding how to recognize and respond to a concussion.
While the Brain and Behavior Clinic does not work with kids under the age of 17, we seek to be a brain health resource for everyone.
We’re Expanding Our Practice
We’re Expanding Our Practice: Offices in Boulder, Denver & Now Colorado Springs
The Brain and Behavior Clinic is excited to announce that after 38 years treating patients in the Denver and Boulder areas, we have opened a new office in Colorado Springs.
Our goal in expanding is to make neuropsychological testing, brain training, trauma and resilience psychotherapy, Slzheimers treatment + neurofeedback more accessible to our patients in the Castle Rock, Colorado Springs, and Pueblo areas.
As the only neuropsychological assessment and treatment practice in Colorado Springs with extensive experience in forensics, we look forward to extending our network of doctors, psychotherapists and brain health practitioners in the area in order to further meet the needs of your community.
Which treatments are virtual and which are in office?
With the onset of the COVID-19 pandemic, we adapted much of our practice into the virtual space, offering initial consultations, therapy sessions, and rehabilitation treatments remotely through a secure telemedicine platform.
Our comprehensive advanced neuropsychological tests measure our patients’ brain function in the areas of attention, concentration, learning, memory, language abilities, executive functioning, motor skills, and emotional status. Our psychometrists are specifically trained to encourage the best performance out of our patients during testing to provide our doctors with the most accurate analysis possible: this is essential to understanding any brain injuries the patient may have sustained, identifying any cognitive conditions that may be present, and developing effective treatments.
Who will my doctor be?
Prior to any neuropsychological testing and for all other treatments, patients will meet their doctor for an initial interview online via our telemedicine platform. For this reason, your location will not affect which of our highly experienced doctors assists you; it will simply be determined by your and our doctors’ availability.
If neuropsychological testing is recommended following your initial virtual visit, you will meet with one of our skilled psychometrists in the office location most convenient for you—whether Denver, Boulder, or Colorado Springs—and undergo paper/pencil testing of your cognitive abilities.
How do I schedule my appointment for any location?
No matter where in Colorado you are located—and whether you are seeking head injury treatment or an age-related brain health check-up—simply give us a call at our main number and we will walk you through the next steps:
We will schedule appointments, get you set up with our telemedicine portal, and provide you with any necessary electronic paperwork. If relevant, we will call your attorney and make all of the appropriate financial arrangements.
The Brain & Behavior Clinic is committed to making high-quality, comprehensive neuropsychological care accessible to everyone, and we look forward to meeting you online or at one of our now three locations throughout Colorado:
Colorado Springs Office: Just northwest of the intersection of N. Academy Blvd and Constitution Ave.
Boulder Office: Just north of downtown on Broadway
Denver Office: Just west of the Mile High Stadium
Visit our website to learn more about our practice, or give us a call to schedule an appointment now:
303-938-9244
Emotional Regulation and Cognition: A Multidirectional Relationship
Emotional Regulation and Cognition: A Multidirectional Relationship
Your brain and body are a dynamic structure that allows—and requires—your physical, mental, and emotional health to work together tridirectionally. When you are emotionally well, your cognition and physical wellbeing benefit—and vice versa. When you are cognitively unwell, your emotional and physical wellbeing suffer—and vice versa.
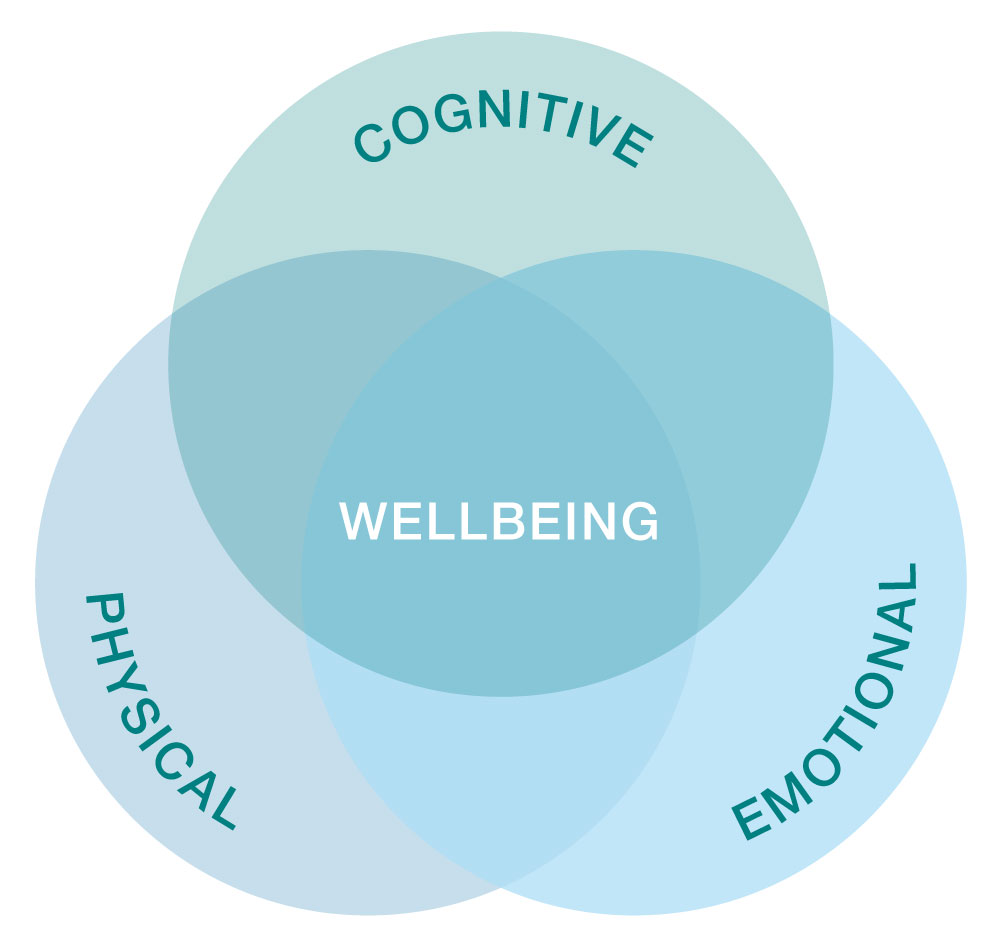
While this fact of complex structures is fairly implicit, it’s easy to overlook the magnitude of influence that each branch of health has on the other—especially when it comes to the less concrete emotional and cognitive branches and the ambiguity that often accompanies depression, anxiety, and other stress disorders.
When a person sustains a traumatic brain injury (TBI)—whether mild or severe—they can experience sudden and lasting cognitive impacts: an experience that can create extraordinary amounts of stress and apprehension.
The prospect of unpredictable but weakened cognitive function creates uncertainty in life as a whole: without the ability to perform at the same level, you may begin to consider the stress-inducing idea that your life will start to fall through the cracks and that you may not be able to sustain the life you’ve built for yourself and/or your family.
Whether as a result of a TBI or a known disorder like Alzheimer’s disease, the need to self-limit due to impaired cognition can lead to major depressive symptoms too.
It’s important to note that experiencing substantial emotional impact when your cognitive function is diminishing is expected and natural—because emotions, just like our physicality and cognition, are a fundamental part of our being as humans.
Of course, just as impaired cognitive function can take a toll on a person’s emotional wellbeing, so can one’s emotional wellbeing impact their cognitive function. In fact, emotional dysregulation can have a substantial impact on attention, memory, and decision-making abilities.
Attention
Depressive thoughts, money stress, worries about the future: they distract your mind and hinder the otherwise limitless bounds of your brain. Thinking requires a lot of energy, and when your brain is navigating adverse emotions, it uses some of this energy, diminishing your capacity to think as hard and maintain focus on the task at hand. With emotional dysregulation, you might find yourself:
- Making simple mistakes at work or at home
- Losing track of time or your surroundings
- Struggling to tune out environmental distractions
- Missing portions of conversation or instruction
- Feeling particularly overwhelmed by challenging tasks
Memory
The distractibility brought on by emotional dysregulation can lead to problematic memory difficulties too. In the face of unusual amounts of stress, depression, or an anxiety disorder, you might find yourself:
- Frequently losing everyday items
- Running late or missing appointments
- Immediately forgetting new information, like a person’s name
- Forgetting parts of a conversation or instructions
- Needing to re-read text
Decision-making
When extra energy is expended on emotional dysregulation and our brain’s attentional capacity is reduced, we have less room for analysis; and even the simplest decisions, like what to wear or where to eat dinner, can feel like challenging deductions. When emotionally dysregulated, you might find yourself:
- Feeling easily overwhelmed
- Taking longer to complete tasks
- Feeling fatigued by activities that require multiple decisions
- Struggling to begin an undefined project
The exacerbated symptoms of the multidirectional relationship between cognitive decline and emotional dysregulation is harmful to the quality of day-to-day life. But not only that, emotional dysregulation can impact long-term brain function too.
A 2019 study showed that repeated depressive episodes weaken both working memory and long-term memory, and another study showed that excess cortisol (that is produced by the brain in response to stress) can impact the hippocampus, which is partially responsible for memory consolidation.
Fortunately, there is so much we can do both to immediately uplift our emotional wellbeing and to enable our brains and bodies to better cope in the face of dysregulation. One way is to build stress resilience, or neuroplasticity. Flexing the brain may sound like an odd or unapproachable feat, but there are a number of very simple neuroplasticity exercises you can integrate into your daily routine that can, especially over time, enhance your brain’s flexibility.
1) Practice communicating your emotions.
To help yourself better understand your emotions, practice talking about the feelings you don’t ordinarily share with others. You can start by sharing, even just once a week, with a trusted friend or partner—or even writing in a journal.
2) Integrate breathwork into your daily routine.
Practice intentional breathing everyday at the same time—right when you wake up or before you go to sleep, for example. Simply commit to a few moments of slow, easy breathing.
3) Meditate to find calm.
Conjure up a childhood memory of a calm and peaceful place in nature. Try to focus on the senses of that memory to build somatic connections. Ask yourself: What did I feel then? What did I see, hear, or smell?
4) Move your body.
Gesture shaking can be a powerful way of externalizing and releasing emotion. Start with one body part, like your arm or leg, and shake it for a few seconds. Repeat this a few times to help your nervous system recalibrate.
Through mental and physical exercises like these, you can begin to strengthen and support your brain. However, in the face of a traumatic brain injury; cognitive disorder; or persistent depression, anxiety, or other stress-related disorder, it’s important to support yourself with additional treatment.
Our team at the Brain and Behavior Clinic can help. We develop personalized treatment plans that address one’s unique set of physical, emotional, and cognitive symptoms to reinstate optimal cognitive function and emotional wellbeing.
Whether you’re struggling with the emotional impact of a cognitive impairment, the cognitive symptoms of an emotional disorder, or both, your experience is valid and your emotional wellbeing matters.
Schedule a consultation with one of our neuropsychologists to learn how we can help you.
What is Traumatic Brain Injury?
What is Traumatic Brain Injury (TBI)?
A traumatic brain injury is any injury to the brain that’s sustained through forceful movement or impact. TBIs can be categorized into three types—mild, moderate, and severe. Moderate and severe TBIs are often marked by initial confusion or loss of consciousness, while mild TBIs—most commonly referred to as concussions—often result in a mere momentary daze, although often manifest later in the form of post-concussion syndrome.
How does TBI occur?
Car accidents and falls are the leading causes of traumatic brain injury—making up more than half of reported cases—but they can occur as a result of fights, sports injuries, or any other occurrence in which the head is struck by an object, pierced by an object, or shaken.
What are the symptoms of TBI?
The symptoms of TBI look different for everyone, and they depend on the degree of head injury; however, no matter the degree, they typically have physical, emotional or behavioral, and cognitive manifestations.
While the particular combination of symptoms is unique to each person who sustains a TBI, it generally is some compound of the following symptoms.
Common physical symptoms:
- Headaches
- Dizziness
- Blurred vision
- Sleep problems
- Ringing in the ears
- Balance difficulties
- Significant fatigue
Common emotional or behavioral symptoms:
- Irritability
- Decreased patience
- Frustration
- Low motivation
- Worry
- Personality changes
- Depression
Common cognitive symptoms:
- Memory difficulties
- Mental inefficiency
- Tendency toward cognitive overwhelm
- Difficulty concentrating
- Speech and word-memory problems
- Limited strategic or organizational thinking
How is TBI Diagnosed?
Because of the diverse range of traumatic brain injuries and the variation in symptom onset, it isn’t always apparent when a TBI has been sustained. If you’ve recently been in an accident and suffered a blow to the head and you’re experiencing any of the above symptoms—or are otherwise experiencing noticeable changes to your health—it’s advisable to see a medical professional right away.
If you are in fact experiencing a TBI, the best thing you can do is seek treatment immediately. The sooner you begin aiding your body in recovery, the better—and more efficiently—your body is able to repair itself.
How do you treat TBI?
If you’re experiencing TBI, it’s important that you limit your activities as you heal. This means refraining from taking on extra jobs and responsibilities, temporarily reassigning some of your current responsibilities, limiting the number of hours you work, and getting enough rest.
Here are a few specific strategies for conserving your energy each day:
- Schedule rest breaks throughout the day.
- When you return home from work, go straight to your bedroom or other private space, and spend 20 minutes resting with your eyes closed—without any distractions.
Do not read a magazine, watch TV, open the mail, pet the dog, talk to your spouse, read your text messages, or fold the laundry. Simply lie down, and rest.
- Hire someone to do your grocery shopping for you; or order in advance online or over the phone.
Here are some strategies for improving your cognitive function as you heal:
- Use a notebook, daytimer, and or mobile app to record important information that you need to remember.
- Carry a small notepad with you wherever you go, and write down new information.
- Wear a watch that beeps every hour to remind you to check-in with your daytimer.
- Ask people to repeat or explain things more simply whenever necessary.
While these methods can provide some relief and help you to cope, it’s important to seek additional treatment—especially if you’re experiencing a moderate-to-severe TBI.
The good news is that there are plenty of treatment options available, including treatment with us at The Brain and Behavior Clinic. We have over 35 years of experience diagnosing, treating, supporting, and advocating for people with traumatic brain injuries.
We’ll work with you to develop a personalized treatment plan that addresses your unique set of physical, emotional, and cognitive symptoms and that gets you back to your optimal brain health and cognitive function.
Schedule a consultation with one of our physicians!
What is Post-Concussion Syndrome (PCS)?
What is Post-Concussion Syndrome (PCS)?
Post-concussion syndrome, or PCS, is a constellation of symptoms that arise and persist after a concussion has been sustained.
A concussion is a mild form of traumatic brain injury (TBI) that occurs when the brain is subjected to trauma—whether struck by an object, pierced by an object, or shaken.
Though the damage incurred from a concussion is minor—and often isn’t perceived by CT or MRI scans—it can still severely impact one’s life by altering multiple aspects of one’s health and causing prolonged physical, cognitive, and behavioral or emotional symptoms.
How can a concussion be identified?
Sudden, violent movements or direct blows to the head often result in a concussion—something that can occur during a number of commonplace accidents, including:
- Car accidents
- Falls
- Fights
- Sports accidents
In the event of a concussion, a person typically experiences a momentary period of confusion, disorientation, or slowed processing. While some experience effects immediately following their head injury, many people don’t notice concussion symptoms until hours or even a couple of days later.
So if you’ve recently fallen, suffered a strike to the head, or been in a car accident that caused whiplash, it’s important to keep a close eye for developing symptoms—even if the immediate aftereffects were minimal.
Why do concussion symptoms occur?
The brain is made up of thousands and thousands of long, thin nerve fibers. If your head is hit hard enough to sustain a concussion, some of these nerves will be torn or broken.
Fortunately, your brain has many other thousands of nerve cells which are not damaged as a result of the injury and which attempt to take over the work of the damaged nerve cells. This reparation work, while healing and necessary, is demanding on the rest of your body; and it results in the compounding symptoms that often occur.
Depending on the scope of the injury and the preexisting health factors that affect your body’s ability to heal, this recovery process can resolve within a couple of weeks—as is typical of a standard concussion—or it can persist for several months. When symptoms persist in this way, beyond about two weeks, post-concussion syndrome is typically diagnosed.
What does post-concussion syndrome feel like?
Because of the highly complex and communicative nature of our brains and bodies, a head injury’s damage to brain cells rarely manifests in an isolated manner and usually induces a combination of physical, emotional or behavioral, and cognitive symptoms.
Of course, every person’s body functions differently, so the particular set of symptoms will vary; but generally a person experiences some combination of the following symptoms.
Physical symptoms may include:
- Headache
- Trouble sleeping
- Sensitivity to light or noise
- Blurred or double vision
- Hearing loss or ringing in the ears
- Dizziness or vertigo
- Nausea
- Loss of smell and/or taste
- Appetite changes
Emotional or behavioral symptoms may include:
- Irritability
- Increased anxiety
- Tendency toward overwhelm
- Depression or lack of interest/motivation
- Personality changes or sudden mood swings
Cognitive symptoms may include:
- Difficulty concentrating or focusing
- Short-term memory loss
- Slowed reactions
- Trouble learning new things
- Difficulty making decisions
- Impaired reasoning
All of these symptoms are expected and treatable, and most people can return to their normal level of functioning within six months of their accident, if not sooner. However, in order to recover fully, it’s important to give your body proper support, and the sooner you seek treatment, the better equipped your body becomes to heal itself efficiently.
Fortunately, treatment is very much available! We at The Brain and Behavior Clinic have over 35 years of experience diagnosing, treating, supporting, and advocating for people with post-concussion syndrome; and we can develop a personalized treatment plan that will not only help you heal, but help you to optimize your cognitive function, too.
Schedule a consultation with one of our physicians. And for some immediate action toward healing, try implementing some restful practices in your daily routine and self-administering these coping methods.
Treating Post-Concussion Syndrome: Compensation Strategies
Treating Post-Concussion Syndrome
If you’ve been in a car accident, fallen headfirst, or otherwise taken a blow to your head, you may have sustained an injury to your brain. Even if you didn’t immediately lose consciousness or experience confusion, as is typical of a moderate to severe traumatic brain injury (TBI), you may have incurred the most common form of mild TBI—a concussion.
Oftentimes, this injury cannot be seen on CT or MRI scans, because the damage is so minor. However, the effects can still severely impact your life in physical, emotional, and cognitive ways; these persisting effects from minor brain damage are what we call Post-Concussion Syndrome, or PCS.
What’s happening when PCS occurs?
The brain is made up of thousands and thousands of long, thin nerve fibers. If your head is hit hard enough for a concussion to occur, some of these nerves will be torn or broken. Fortunately, your brain has many other thousands of nerve cells which are not damaged as a result of the injury and which attempt to take over the work of the damaged nerve cells.
During the first few months after the injury, the brain works to heal itself, just like your body works to heal a bruise on your arm. As your brain and body conduct this hard work, symptoms are felt not only physically, but emotionally and cognitively, as well. Fortunately, there are a number of strategies you can use to ease your symptoms, compensate for your limited capacities, and assist your body in recovery.
How can I treat the symptoms of PCS?
Every person’s experience with PCS looks different, and depending on your overall health and the particular cause of injury, the symptoms will vary. So, let’s address these healing strategies as they relate to each potential symptom.
Here’s what you can do:
If you’re experiencing memory problems:
- Use a notebook, calendar or daytimer to keep track of important information. Carry it with you at all times.
- Record appointment times.
- Note the names of new people.
- (Use a cueing system to help remember their names—a description of the person, for example.)
- Write down all important information, such as questions you want to ask healthcare providers or information you want to share with your family.
- Make use of alarms or timers to remind you when it’s time to do certain tasks.
- Use several modalities when memorizing—say it loudly, visualize it and write it down.
If you’re struggling with attention and concentration:
- Organize your environment as much as possible.
- Minimize visual and auditory distractions, such as television and radio.
- If you have to work in a noisy environment, try wearing earplugs.
- When at work, keep your door closed.
- When driving, keep the radio off.
If you’re feeling overwhelmed or are lacking motivation:
- Make a daily schedule. Check off activities as you complete them.
- Break large tasks into small ones.
If you’re experiencing perceptual problems or processing information more slowly:
- Write down and repeat back verbal information, such as directions and phone numbers.
- Allow more time to complete activities.
If you’re experiencing fatigue:
- Schedule breaks throughout the day for rest.
- Complete especially cerebral activities in the morning or early afternoon.
- Exercise daily.
- Focus on improving sleeping habits.
- Maintain a balanced diet.
- Set limits on your energy output.
How will these strategies aid recovery?
You may experience the above symptoms all at once, or you may notice their development over the course of several weeks or months. As you experience a new symptom, try the correlating, self-supportive tools. It’s incredible the recovery the body can achieve with some support.
By the time six months have passed since your accident, you should be feeling very close to normal. But employing these assistive strategies can allow you to achieve much higher functionality along the way, and may quicken your recovery time.
How can The Brain and Behavior Clinic help?
Beyond these self-administered methods, the Brain and Behavior Clinic can, with our research-based approach and years of experience, develop a personalized treatment plan that holistically addresses physical, emotional, and cognitive symptoms to most effectively minimize the effects of post-concussion syndrome on daily life.
Learn more about BBC’s treatment plans, or schedule a consultation with one of our doctors.